3D printing is an important technology that emerged in the 1980s and has developed rapidly in the past 30 years. 3D printing technology is different from traditional cutting and casting technology: not only makes the physical structure of the product change, but also can be customized according to individual needs, to achieve a perfect match between the material and the lesion, and can carry cells and biologically active microspheres. In situ printing of the bone defect site. These characteristics determine the broad application prospects of this technology in the field of biomedicine.
This paper aims to outline the principles of 3D printing technology and its application in orthopedics, and to provide an outlook for its future development. The goal is to deepen the clinician's understanding of 3D printing technology, but also to facilitate its clinical transformation and provide patients with better medical services.
First, what is 3D printing technology
3D printing technology is also known as "rapid prototyping" or "additive manufacturing".
Additive manufacturing technology is a technique for constructing objects by means of "layered manufacturing, layer-by-layer stacking" based on digital model files and applying adhesive materials such as powdered metal or plastic. It includes SLA, SLS, and 3DP. , FDM, etc.
In order to facilitate understanding and promotion, the media will also refer to additive manufacturing technology as 3D printing technology. Additive manufacturing technology was first used primarily for the design of prototypes, so it is also known as rapid prototyping.
For more than 30 years, 3D printing has generally been used to create physical models through data software. In the past 10 years, with the development of 3D printing technology, the cost of 3D printers has been greatly reduced, and its application range has been expanded. It has been applied to teaching, medical and scientific research fields.
Medical 3D printing mainly includes the following four processes:
1 collection and dataization of printed image information;
2 processing and conversion of image data information;
3 using data information for 3D printing;
4 Post-processing and performance evaluation of printed matter.
(1) Collection and digitization of printed image information
The parts to be printed are photographed by X-ray, CT and MRI, and the obtained image information is digitized, and then exported in the "DICOM" format commonly used by medical imaging software.
Since the resolution of medical images is much larger than the resolution of 3D printers, the data information obtained by medical imaging is sufficient to meet the accuracy requirements of 3D printers [2].
(2) Processing and conversion of image data information
The image data information of the printed matter also needs to be processed according to the final printing needs. Data processing software commonly used in the medical field are Mimics software (Materialise, Belgium), UG Imagewa software (EDS, USA) and Geomagic Studio software (Geomagic, USA).
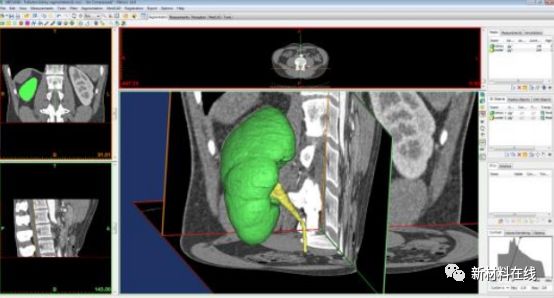
Image source: Network public information
(3) Using data information for 3D printing
The 3D printer can reconstruct the printed matter based on the data in the "STL" format. The general FDM technology 3D printer print accuracy of up to 0.2 mm, while the SLA technology can be accurate to 0.025 mm, with higher printing accuracy, and is now in mass production.
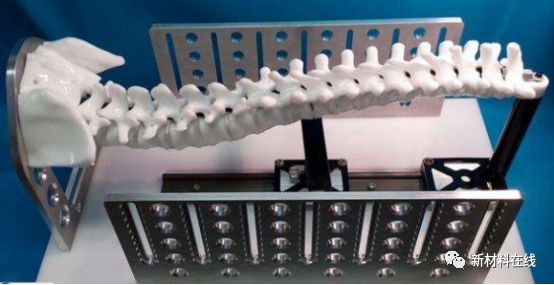
Image source: Network public information
(4) Post-processing and performance evaluation of printed matter
Sometimes it is necessary to post-support the printed matter, smooth surface, quenching and tempering of metal parts, and some mechanical processing can be performed if necessary to compensate for the limitations of the printing process. At the same time, the processed printed matter is evaluated according to its use, such as metal phase analysis, material surface inspection, kinematics analysis and finite element analysis.
Second, the application of 3D printing in orthopedics
(1) Techniques and materials commonly used in orthopedic 3D printing
3D printing technology eliminates the need for industrial molds, produces very little waste, and has a small gap between individual production and batch production costs. Therefore, it has obvious cost and efficiency advantages in non-batch production, greatly simplifying the process from design to product physical. The most common molding methods currently directly related to orthopedics include:

Figure 1 Common orthopedic 3D printing method
At present, the materials used for 3D printers are gradually increasing, including natural medical materials such as collagen and chitosan, synthetic polymer materials such as polylactic acid, polyglycolic acid and polyetheretherketone, bioactive ceramic materials such as hydroxyapatite, and titanium. Medical metal materials such as alloys. The choice of printed materials is closely related to their use.
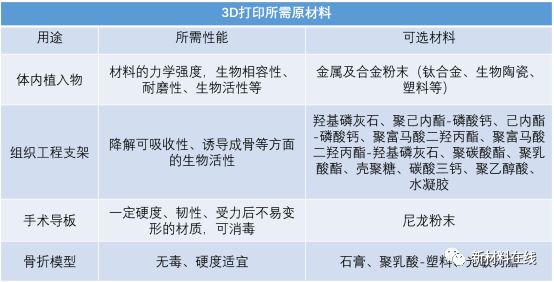
Figure 2 3D printing using raw materials
(B) the application of 3D printing in orthopedics
1. Preoperative planning
For fracture patients, especially those with complex fractures, preoperative physical anatomical models for analysis or simulation of surgical procedures are more instructive than MRI or CT scans that rely solely on two-dimensional planes (Figure 2).
Preoperative application of 3D printing technology can make doctors have a more intuitive understanding of the patient's condition, especially for young doctors with insufficient experience, which is more conducive to the diagnosis and treatment of diseases.
The clinical results show that the 3D model group has shorter operation time, less intraoperative blood loss and postoperative drainage than the non-3D model group, which is conducive to accurate reduction of fracture, improve surgical precision, shorten operation time and achieve better surgical results. .
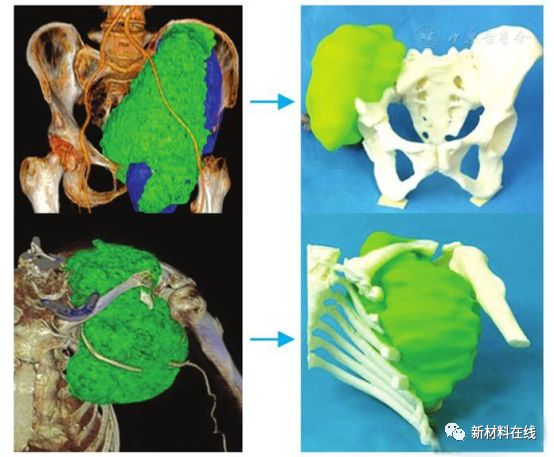
Figure 3 Pelvic (upper) and shoulder (lower) malignant bone tumors were preoperatively planned using 3D printing techniques. Print a tumor model showing the tumor resection boundary
Image source: Network public information
[Medical application] In January 2016, Professor Wang Guihuai, director of neurosurgery at Chang Gung Hospital, Tsinghua University, Beijing, performed a scene of “Waltz on the tip of the knife†in neurosurgery. He used 3D printing technology to “clone†the lumbar model of the patient's lesion and accurately present it. The distribution and morphology of the patient's tumor and vertebral body, blood vessels and ureters were accurately performed, and tumor resection was performed accurately.


Image source: material person
2. Making a surgical navigation template
The surgical guide is called "surgical navigation physical template". The main function is to help the accurate reduction of the fracture, the auxiliary screw and other implants or instruments reach the predetermined position. While improving the convenience of the operation, the perforation rate and the direction error can be reduced. The rate makes the accuracy of the surgical operation significantly improved.
The use of 3D printed surgical guides in the adjuvant treatment group with high accuracy of pedicle screw placement, reduced intraoperative risk, high surgical safety and satisfactory clinical efficacy is an effective and worthwhile technology.
The application of surgical guides makes medical treatment more precise, in line with the current concept of precision medicine, which can improve the surgical treatment while reducing the damage of patients.
[Medical application] In April 2015, Xiangya Hospital of Central South University successfully implemented a complicated orthopedic surgery. Pre-operative exercises and program development were performed using a fine 3D printed model.
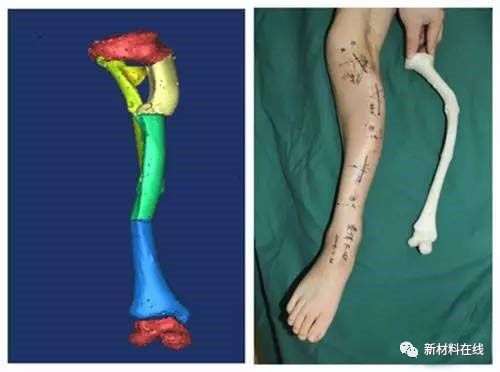
Figure 4: Walkthrough and scenario development using a fine 3D printed model
Image source: Network public information
3. Customized personalized prosthesis and internal plants
Prostheses and endophytes are often used in the repair of bone and joint injuries. Traditional prostheses and internal plants have fixed specifications. Surgical knives and electric drills are needed to trim the grafts in the surgery to give us the shape and size we want, while 3D printing can be tailored to patients. s material.
In terms of the bio-fixation mode of the stent, the fixation of the stent to the surrounding tissue is divided into two types: bone length and bone length.
The pattern of bone length fixation is that the bone is wrapped around the surface of the implant. The common surface of the implant has a rough surface, a sintered surface, a plasma sprayed surface, etc. The bone grows into a fixed pattern for the growth of the bone tissue. Internally, it forms a solid whole with the inner plants.
Both of these fixation methods significantly affect the stability and end-life of the prosthesis and endophytes in the patient.
Promoting the formation of bone ingrowth maximizes the life of the prosthesis, and 3D printing technology has advantages over traditional methods in making porous implant materials that are beneficial for bone ingrowth.
Many common implants use tricalcium phosphate material. Mixing magnesia or strontium oxide in a porous tricalcium phosphate scaffold will be more beneficial to bone growth. Studies have also shown that porous titanium alloy implants have good bone ingrowth ability, can promote bone healing at the prosthesis-bone interface, thereby prolonging the service life of the prosthesis.
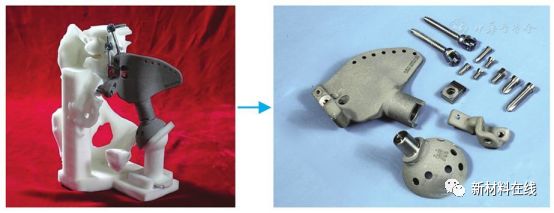
Figure 3 Making a personalized hip prosthesis with 3D printing
Image source: Chinese Journal of Orthopaedics
[Medical application] In February 2015, Xiangya Hospital of Central South University successfully implemented a reconstruction of the jaw bone using a 3D printed titanium metal grid structure.
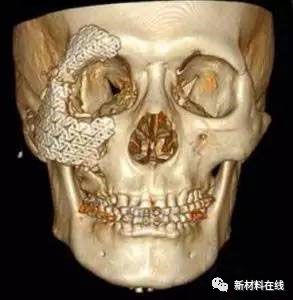
Figure 4 Jaw reconstruction using a 3D printed titanium mesh structure
Image source: Network public information
4. Custom external fixing bracket
Research on orthopedic external fixation brace materials has been the most basic and active area of ​​trauma treatment.
From the initial splint to plaster bandages, thermoplastic splints, removable foam splints, and polymer splints, the invention and application of these devices have led to a more effective approach to the treatment of traumatic orthopedic patients.
The external fixation material is directly in contact with the patient's limb. Therefore, the ideal external fixation brace should have the following characteristics: 1 stable but not too hard, to prevent soft tissue damage and affect the later functional recovery; 2 as close as possible to the patient's soft tissue shape; 3 wear time Long, should be as light as possible and washable.
3D printing technology can make up for some defects in the manufacture and use of existing external fixing materials.
[medical application]
1. Plastic surgery: burn treatment, facial reconstruction, personalized customization of rhinoplasty and sacral prosthesis, personalized repair of skull defect, mandibular reconstruction and osteotomy.
2. Stomatology: personalized customized invisible orthodontic appliances, dental inoculation

Image source: Network public information
3. Rehabilitation aids: hearing aids, personalized orthopedic exoskeletons.

Image source: Network public information
4. Development of new surgical instruments
In order to better meet the needs of personalized medicine, adapting to the use of personalized materials, it is necessary to match the personalized surgical instruments, and 3D printing makes it possible. George and other SLS technology to print surgical instruments, including hemostatic forceps, needle holders, surgical handles, hooks, tweezers, etc., through the simulation of human corpses and inguinal hernia repair and evaluation of postoperative ergonomic function findings, and tradition Compared with surgical instruments, 3D printed surgical instruments can greatly reduce the production time of personalized surgical instruments without increasing costs.

Image source: Network public information
5. Tissue engineering scaffold
The purpose of tissue engineering is to generate alternative tissues or organs in vivo or in vitro to repair the function of damaged tissues and organs.
Seed cells, bioactive factors and scaffold materials are the three major elements required for classical tissue engineering construction.
The ideal stent should have the following characteristics: 1 good biocompatibility; 2 moderate biodegradability; 3 ability to induce or guide tissue regeneration; 4 have certain biomechanical strength and plasticity; 5 non-toxic and non-immunogenic 6; has a suitable pore size; 7 can provide cytokines required for cell growth and differentiation, such as vascular endothelial growth factor, bone morphogenetic protein and the like.
The 3D printing technology can better achieve the above features compared to the conventional technology.
Zhu Xiang et al. used silk fibroin and collagen as raw materials to make artificial bionic spinal cord catheters, which were placed under the skin of SD rats and completely degraded after 4 weeks. Neural stem cells can grow in the pores of artificial bionic spinal cord catheters, which are spherical or fusiform; densely growing on the surface of the catheter, and some cells stick out of the pseudopod to the surface of the catheter.
Ding et al. used 3D bioprinting technology to print the osteochondral biphasic scaffold. The biomechanical properties of the regenerated bone and cartilage tissue were close to the normal state, and the bone-cartilage interface was good.
Li Xiang et al found that the porous titanium/chitosan/hydroxyapatite (Ti/Ch/HA) composite structure can match the mechanical properties of human bone tissue, and is more suitable for the adhesion growth of osteoblasts than simple porous titanium. An ideal replacement for bone defect repair in load-bearing parts.
Using polyacetic acid and chitosan as raw materials, Lee et al. constructed individualized mandibular condyle scaffolds by 3D printing technology and applied apatite coating on the surface of the material. The scaffold not only supports cell growth, but also promotes bone ingrowth and bone conduction.
Melke et al. found that silk fibroin scaffolds have osteogenic potential in vivo. The above studies were carried out in small animals, and whether they have the same effect in the human body remains to be further studied.
6. Drug development, release and dosage form
3D printing technology has been used in the development and preparation of drugs and will have a huge impact on the field.
The advantages of 3D printing include precise control of microdroplet size and dose, high reproducibility, and the ability to make pharmaceutical dosage forms with complex drug release models. Complex production processes can also be standardized using 3D printing to make it simpler and more feasible.
3D printing technology has been used to print many novel dosage forms such as microcapsules, artificial hyaluronic acid extracellular matrices, antibiotic printed micrographs, mesoporous bioglass scaffolds, nanosuspensions, multi-layer drug delivery devices, and the like. The 3D printed pharmaceutical ink formulation includes a variety of active ingredients, including steroidal anti-inflammatory drugs, acetaminophen, theophylline, caffeine, vancomycin, ofloxacin, tetracycline, prednisone, paclitaxel, folic acid, and the like.
Li Cheng et al. can promote the repair of articular cartilage damage and inhibit the progression of osteoarthritis by intra-articular injection of hyaluronic acid-chondrogenic morphogenetic protein-1 microspheres into rabbits. Ko et al. demonstrated that sulforaphane-polylactic acid-glycolic acid copolymer microspheres are an effective injectable delivery system that can be used to treat osteoarthritis.
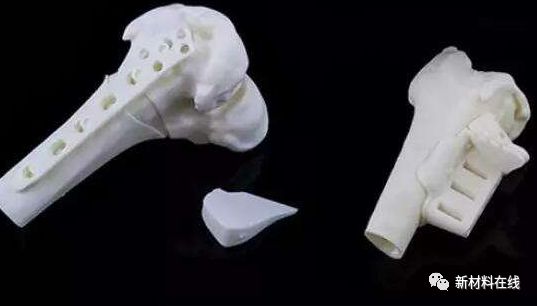
Image source: Network public information
Third, thinking and outlook
Despite the advantages of personalization and diversification of printed materials, there are still some unavoidable problems in the development of 3D printing.
1 The development of printing materials is the difficulty and core of the development of 3D printing technology. At present, the metal material commonly used in orthopedic instruments is titanium alloy powder, which is affected by the particle size distribution of the material, the bulk density (the mass of the powder freely filled per unit volume under the specified conditions), the oxygen content, the fluidity and the like, and other metal materials and The printing technology of polymer materials is still in the experimental stage. Research on how active printing materials maintain cell activity and its function is still at the bottleneck stage.
2 In the application of tissue engineering scaffolds, the optimum degradation rate, mechanical properties, porosity and pore size of 3D printed bone tissue engineering scaffolds are inconclusive. At the same time, after the drug microspheres were loaded on the stent, the complete matching of the degradability, osteogenicity and drug release performance of the stent was still in the preliminary experimental stage. The resolution of the current 3D printer is micron level, and the ultrastructure of the bone is nano level, so it is also necessary to improve the resolution of the 3D printer to improve the function of the bracket.
3 In terms of printing organs, only a single active cell can be used to print tissues and organs. The regenerated organs and tissues are small-scale and relatively simple, often avascular, non-neural, lymph-free, relatively weak, hollow or The main blood vessels are required to provide nutrition. However, the intraosseous vasculature can supply oxygen and nutrients to tissues within 100 μm of the blood vessels.
Some scholars have observed that when the thickness of the constructed tissue exceeds 100-200 μm, the oxygen supply limit between the host and the graft will be exceeded. Therefore, to print complex organs and tissues, it is necessary to construct a precise multicellular structure with a vascular network. The related research can not achieve this purpose, and can not replicate the complexity of human tissue and organ function.
4 expensive, high threshold. Although the price of 3D printers has gradually declined in recent years, good 3D printers are still expensive, plus related CT, MR equipment, modeling and reverse engineering, CAD software, etc., with higher investment. In addition, the use of equipment and software requires specialized technical training or multidisciplinary, multi-disciplinary professional and technical personnel to work together.
5 need the combination of clinicians and engineers (healing workers combined), the only way to scientifically design 3D surgical solutions, manufacturing accurate 3D implants, truly reflect the application value of 3D printing technology in orthopedics, and better benefit patients.
Projector Lamp,Projector Light Bulb,Projector Lamp Replacement,Projector Bulb Replacement
Shenzhen Happybate Trading Co.,LTD , https://www.szhappybateprojectors.com